Abstract
Background: Select inherited thrombophilias have been shown to potentiate the risk of venous thromboembolism (VTE) during pregnancy and the post-partum period. Sickle cell trait (SCT) is associated with an increased risk of VTE in the general Black population; however, prior studies investigating the risk of pregnancy-related VTE among women with SCT have been limited by an overall low number of VTE events. We, therefore, designed a retrospective cohort enriched for pregnancy-related VTE events among Black women at Johns Hopkins Hospital to address this question.
Methods: We generated a cohort enriched for pregnancy-related VTE at Johns Hopkins or affiliate hospitals from 2009-2019 by using EPIC and an internal ObGyn database to identify Black women ≥18 years with at least 1 pregnancy encounter in addition to at least 1 VTE-related ICD-10 diagnosis code or comprehensive VTE-related search term. All charts were manually reviewed to confirm hemoglobinopathy status and to verify the presence or absence of a VTE event during pregnancy or 6 weeks post-partum. Individuals with sickle cell disease, history of VTE prior to index pregnancy, catheter-related or superficial vein thrombosis only, or unknown pregnancy VTE outcome were excluded.
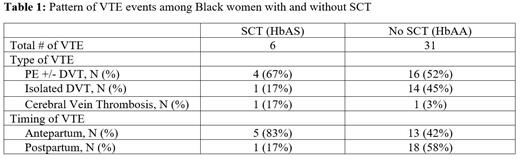
Results: A total of 418 women were included for analysis. The mean age at pregnancy was 30 years (range 18-48), and the prevalence of SCT was 6.7%, which is similar to the prevalence in the general Black American population. Thirty-seven women (8.9%) were confirmed to have a pregnancy-related VTE event. Among those with VTE, SCT carriers demonstrated a higher proportion of pulmonary embolism (PE), unusual vein thrombosis, and antepartum VTE events compared to women with HbAA (Table 1), though numbers were small. After adjusting for age, the risk of VTE was 2.9-fold (95% CI 1.1-7.9) higher among pregnant Black women with SCT compared to those without.
Conclusions: In this enriched cohort, SCT was associated with an increased risk of pregnancy-related VTE among Black women. The pattern of pregnancy-related VTE was different in individuals with SCT compared to those with HbAA, with SCT demonstrating a higher proportion of PE and antepartum events. The higher risk of PE compared to isolated DVT is similar to the pattern observed in prior population-based studies of SCT. Because the prevalence of SCT is high and the overall risk of VTE in pregnancy is low, future studies are needed to determine whether routine thromboprophylaxis is warranted for select high-risk pregnant women with SCT.
Lanzkron: Novartis: Research Funding; CSL Behring: Research Funding; Shire: Research Funding; Novo Nordisk: Consultancy; Imara: Research Funding; Bluebird Bio: Consultancy; Pfizer: Current holder of individual stocks in a privately-held company; Teva: Current holder of individual stocks in a privately-held company; GBT: Research Funding. Naik: Rigel: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal